Corneal Cross-Linking is a procedure that is done to treat a warped or weakened cornea. Surgery or disease sometimes harms the eye’s collagen, which helps keep the cornea together. The cross-linking procedure helps the new collagen fibers unite, strengthen, and reinforce the cornea.
Who Needs Corneal Cross-Linking?
There are some different conditions where cross-linking can be helpful.
Keratoconus: If you have keratoconus, the cornea thins and changes shape over time. The cornea is typically round but will bulge outward until it’s shaped more like a cone if you have this eye condition. This can cause blurry vision and other symptoms. Cross-linking is the only treatment that can be used to stop progressive keratoconus from worsening. This surgery can help you avoid a corneal transplant in the future, which is major surgery.
Corneal Bulging after LASIK Surgery: During LASIK surgery, the corneal tissue is removed to correct blurry vision. It’s rare, but surgery and tissue removal sometimes weaken the cornea. This then causes the cornea to bulge forward, like keratoconus.
The procedure may not be suitable for some people. Your eye doctor can tell you if the treatment can help you since it can’t reverse any cornea changes. Since it does help slow progression, you’ll want to make sure you talk to your eye doctor sooner rather than later if you have keratoconus.
More about Keratoconus
The name keratoconus means cone-shaped, and the abnormal shape of the cornea is what is responsible for the distortion of visual images. If you have keratoconus, you may notice symptoms such as glare, light irritation or sensitivity, distortion or blurring of vision, and frequent changing of contact lens prescriptions or glasses with a high level of astigmatism. These symptoms are common for other eye diseases, so getting a proper keratoconus diagnosis from your ophthalmologist is crucial.
The cause of keratoconus is unknown, but it will usually start to appear in people in their late 20s. The disease will usually progress for about 10 to 20 years, and the cornea will continue to steepen. Both eyes may be affected, but one eye will usually be worse than the other. Genetics may contribute to the risk of developing the eye condition. Vigorous eye rubbing helps add to the progression of the disease, so it’s important to avoid rubbing the eyes too hard.
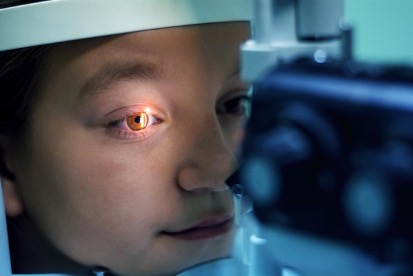
Keratoconus can be seen during routine eye exams, so it’s essential for optimal eye health to regularly visit your eye doctor, especially if you have vision issues. A keratoconus diagnosis will often be confirmed using cornea photographs taken during an exam to highlight any irregularities and a measurement of the cornea’s curvature.

How to Prepare for the Procedure
On the day of the procedure, you shouldn’t wear any aftershave, perfume, or eye makeup. In many cases, you should be able to drink fluids and eat a light meal before the procedure. Since your eyesight will be affected for some time after the procedure, you will need someone to drive you home.
What Happens During the Procedure?
This procedure is outpatient, so you will go home the same day. There are a few things you can expect to happen.
The procedure begins with you being given eye drops to numb your eyes. Your ophthalmologist will then remove the thin outer layer of the cornea. This allows the numbing medication and the other medication to reach further into the cornea, so you won’t feel any pain during the procedure. Then Vitamin B, also known as riboflavin, eye drop medicine is applied to the eye for about 30 minutes. The whole procedure takes about 90 minutes, but you will likely be in the office for two hours to prepare as well as recover.
After applying the medication to the eye, a special device shines a focused beam with UV light rays at the cornea for about 30 minutes. The UV light activates the medicine in the cornea to form new bonds between the fibers in the cornea. Then a bandage is placed over the eyes to help the cornea heal. Your eye doctor will recommend leaving this bandage on the eye for about a week. You will be given steroid, and antibiotic drops to ensure your eye heals properly.
Due to the numbing drops, you shouldn’t experience any pain during the procedure. There can be some pain in the immediate recovery period, though. The bandage reduces discomfort and pain, and you may be prescribed some painkillers after the procedure if over-the-counter pain pills aren’t strong enough.
Types of Corneal Cross-Linking
This procedure has two different types: epi (short for epithelium, the other layer of your cornea) off and an experimental epi-on procedure.
Using the epi-off technique, your eye doctor removes the epithelium before any eye drops are put on. With the epi-on procedure, your eye doctor will loosen the epithelium with a sponge or eyedrops before the eye drops are put in.
What Happens After the Procedure?
During the first week, your eye will be healing, so you should not rub or touch your eyes, get any water in the eye, use makeup around the eye, be in any dusty or smoky place, or do any heavy exercise. Use the eye drops given to you to help your eye heal and follow all instructions from your eye doctor.
Some common side effects from the surgery include being sensitive to light, having a blurry or hazy vision, having dry eyes, feeling mild eye pain or discomfort, and feeling like something is in the eye. Some more severe side effects that are rare include loss of vision, infection, scarring, or worsening of keratoconus.
Even though vision will be blurry, it improves after two to three weeks. If there is a sudden loss of vision, changes in vision, or severe eye pain, it’s important to contact your doctor immediately. There will be no change in the appearance of your eyes.
You will likely be told to stop wearing any hard contact lenses before surgery, and then once the surgery is completed, you will probably not be allowed to wear your lenses for about one month. Each case can be different, so it’s always important to follow any instructions from your eye doctor.
Risks of the Procedure
Just like with other surgical procedures, there are risks involved with Corneal Cross-Linking. Since the procedure removes the epithelium, risks can include delayed healing, corneal epithelium defect, or epithelial haze. Some other risks can consist of infections, keratitis, blurred vision, the appearance of white lines in your field of vision, scarring, or severe inflammation in the eye. Even though there are risks associated with the procedure, there is a low rate of risk and other complications. You should always talk to your eye doctor about any concerns you have.
Recovery Time for Corneal Cross-Linking
Your eye doctor can tell you when it will be safe to resume your normal activities. Most people can resume normal daily activities within one or two weeks after the procedure. However, it’s important to note that your vision may not be stable for several months. This means that your vision, even with contacts and eyeglasses, will change during this time. After six to eight weeks, your eye doctor will likely give you a new prescription for hard contact lenses or refit your glasses.
The goal of the procedure is to keep the corneal bulging from worsening. Unfortunately, it can’t make the existing corneal thinning or bulging return to normal.
Contact Florida Eye Specialists & Cataract Institute
Corneal Cross-Linking is not a procedure you want to put off if you suffer from cornea bulging or keratoconus to preserve your eye health. Since it’s the only approved treatment for keratoconus and can help slow down progression, you want to speak with your eye doctor as soon as possible. Florida Eye Specialists & Cataract Institute is dedicated to eye care with the most advanced technologies in a convenient location. Make an appointment with our specialists today.