There are many diseases that can affect the cornea, causing pain or loss of vision. Disease, infection or injury can cause the cornea to swell (called “edema”) or degrade (become cloudy and reduce vision). Common diseases and disorders that affect the cornea include:
Allergies
Eye allergies are a common condition that affects up to 50 million Americans, causing redness, tearing and many other symptoms that can impair a patient’s vision and affect their overall quality of life.
Patients with eye allergies often experience:
- Red, itchy eyes
- Runny nose
- Sneezing
- Coughing
- Headache
- Sore throat
- Fatigue
These symptoms are caused by triggers in the air, such as pollen, mold, dust or pet dander; or by certain foods or medications, which can cause a different type of allergy. These triggers affect the conjunctiva, the clear layer of skin over the eyes that is similar to the area of skin on the inside surface of the nose, another common source of allergy symptoms.
Treating eye allergies can most effectively be done by avoid the specific triggers that cause your symptoms. If avoidance is not possible, patients can apply cold compresses to the eyes or use artificial tears or over-the-counter medication to relieve symptoms. Prescription eye drops or oral medications may also be recommended to relieve symptoms of eye allergies.
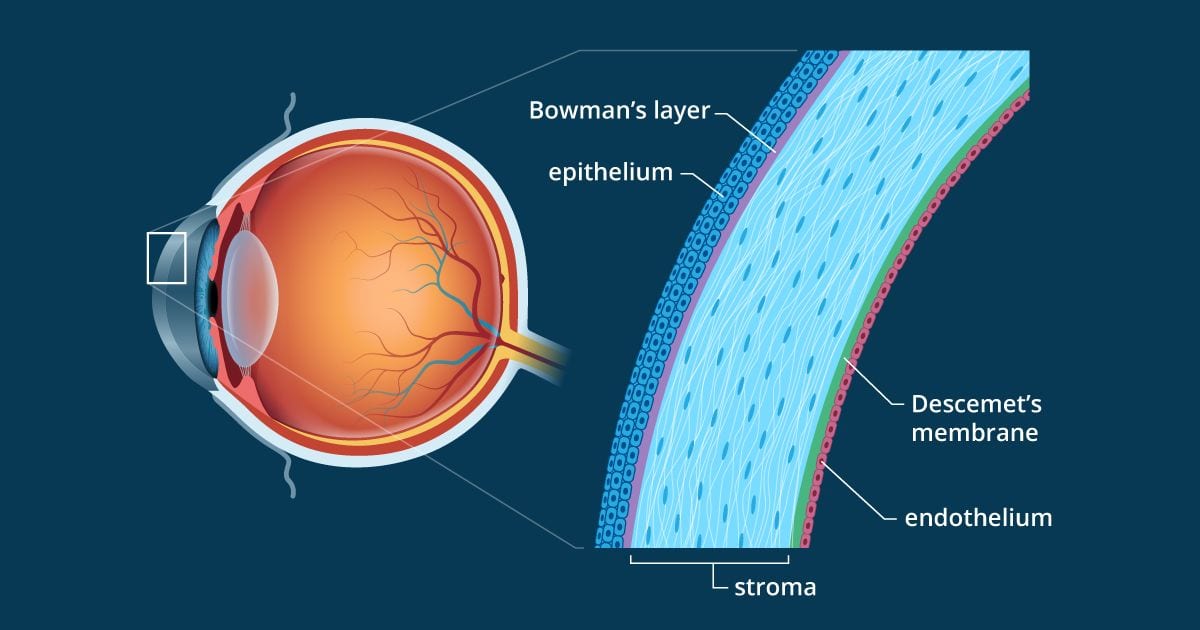
Bullous Keratopathy
Bullous keratopathy is an eye disorder that involves an inflammation of the cornea. This swelling is caused by a problem with the endothelium, which is the inner portion of the cornea, that results in a dysfunction of its pumping system. It may be due to the development of glaucoma, trauma to the area or as a complication of eye surgery. Common symptoms of bullous keratopathy include excessive tearing, light sensitivity and a decrease in visual acuity. In some cases, it may be quite painful.
Bullous keratopathy will typically be treated initially with conservative measures such as eye drops or contact lenses. In many cases, however, those treatments can only provide temporary relief. When bullous keratopathy requires surgery, a corneal transplant is often the most effective way to correct the condition. The newest forms of transplantation remove and replace only the damaged layers of the cornea, preserving more natural eye tissue and speeding recovery.
Corneal Dystrophies
Corneal dystrophies describe a number of eye conditions in which abnormal material builds up on the cornea. When these substances accumulate too greatly, light cannot be focused properly, which affects images being processed by the brain. Most corneal dystrophies are inherited and involve both eyes. Some patients experience no symptoms at all, while others face extensive vision loss, pain, light sensitivity or a scratchy feeling as if a particle is in the eye.
There are more than 20 different types of corneal dystrophies. Some of the most common ones are Fuchs’ dystrophy, keratoconus and lattice dystrophy. The majority of corneal dystrophies progress slowly, starting in one layer of the cornea and sometimes advancing to other layers over time.
Treatment of corneal dystrophies will depend on the condition diagnosed and the severity of its symptoms. In many cases, conservative measures will be initially used, such as wearing special contact lenses that can protect the cornea. For some patients with corneal dystrophies, a corneal transplant may eventually become necessary to restore vision.
Infections
Eye infections can occur when you have been exposed to a virus or bacterium. Different types of infections strike particular portions of the eye. Both eyes or only one may become infected. Common symptoms of an eye infection are red or itchy eyes, pain, discharge, inflammation in the eye area and vision difficulties.
Two of the most typical forms of eye infections include conjunctivitis, otherwise known as pink eye, and styes. Conjunctivitis is an infection of the conjunctiva, the membrane that lines the eyelid and covers the white part of the eyeball. It produces inflammation that affects the blood vessels and gives the eye a pink or red appearance. Styes are small red bumps that develop along the eyelid as a result of an infection. They may cause pain, swelling and tearing of the eye.
Treatment for an eye infection will vary depending on its cause. Some may go away on their own, while others will require the use of warm compresses, over-the-counter medications or antibiotic eye drops. Patients should avoid wearing makeup or contact lenses until after the infection is gone.
Keratitis
Keratitis is an inflammation of the cornea that often develops as the result of an infection, but can also be caused by a small scratch or prolonged contact lens wear. Patients with keratitis may experience redness, eye pain, excess tears, blurred vision and sensitivity to light, depending on the cause and severity of the condition. It is important to see a doctor for a complete eye exam in order to detect any infections at the first sign of symptoms.
If left untreated, keratitis can lead to serious complications and can permanently affect vision. Treatment of keratitis depends on the cause, but may include antibacterial, antifungal or antiviral medications, patching or corneal transplant for severe cases. Your doctor will recommend a personalized treatment plan based on each patient’s individual condition.
Keratoconus
Keratoconus is a progressive eye disease in which the normally round cornea thins and begins to bulge into a cone-like shape. The cornea is the clear, central part of the surface of the eye. In patients with keratoconus, the cone-shaped cornea deflects light and causes distorted vision.
Keratoconus often begins to develop between the teen years and the early 20s, although it can develop at any age. Changes in the shape of the cornea occur gradually, usually over several years. Patients with keratoconus often experience blurred and distorted vision, nearsightedness, and a glaring sensitivity to light.
Early stages of keratoconus can be treated with eyeglasses or soft contact lenses. For progressive keratoconus, treatment methods include rigid gas-permeable contact lenses, and collagen cross-linking (light-activated vitamin eye drops). If keratoconus persists, corneal transplant surgery can be performed to correct the condition.
Ocular Herpes
Ocular herpes is a disease of the eye caused by infection with the herpes simplex virus. Usually affecting only one eye, common symptoms of ocular herpes include inflammation, redness, tearing and sensitivity to light. In severe cases, it can scar the cornea and result in significant vision loss or blindness.
There is no permanent cure for ocular herpes. Once a person experiences an outbreak, there is a good chance the condition will recur. The next time, the herpes symptoms might appear several weeks later or it may remain dormant for years before another flare-up occurs.
Treatment for ocular herpes often involves the use of antiviral eye drops, oral medications or corticosteroid eye drops.
Pterygium
Pterygium is a benign growth of the conjunctiva (lining of the white part of the eye) that grows into the cornea, which covers the iris (colored part of the eye). It can eventually lead to impaired vision.
Patients with pterygium often first notice the condition because of the appearance of a lesion on their eye or because of dry, itchy irritation. Other symptoms include dryness, redness, irritation, inflammation, and tearing. In more severe cases, the pterygium grows over the pupil and limits vision.
The most common pterygium treatment is eye drops (artificial tears) and use of sunglasses. In more severe cases when vision is impaired, surgery may be recommended.
Shingles
Shingles is a condition caused by the varicella-zoster virus, which is responsible for chickenpox. Commonly resulting in rashes on one side of the body, shingles can also affect the eyes. The virus can remain in the body for many years and will occasionally strike the nerves around the eyes. This often produces extreme pain on one side of the face, a rash or redness developing in the eye region or on the forehead, eye redness, inflammation of the eye and vision problems. If left untreated, ocular shingles can lead to scarring, glaucoma or major vision loss in some patients.
Shingles of the eye is often successfully treated with antiviral eye drops or pills to be taken orally. However, if the medication is not taken within the first few days of the appearance of symptoms, it may not be effective. In some cases, steroid eye drops may be prescribed as well to relieve swelling.
Stevens-Johnson Syndrome
Stevens-Johnson Syndrome is a rare condition involving a severe adverse reaction to certain medications or infections. It may begin with symptoms similar to those of the flu, and can lead to skin loss or death if left untreated. Stevens-Johnson Syndrome frequently involves the eyes, resulting in inflammation, irritation and dryness. In some cases, damage to the tissue of the conjunctiva or cornea may be severe, causing scarring and ultimately blindness.
Treatments for ocular problems relating to Stevens-Johnson Syndrome typically involve clearing up infections that result from the condition and keeping the eyes well lubricated through the use of ointments or artificial tears. Some patients may require special contact lenses to protect the eyes from developing corneal abrasions due to changes the condition produces to the eyelids and eyelashes. For other patients, a corneal transplant or amniotic membrane transplant may be necessary to preserve vision.
With a comprehensive eye exam, our highly-trained and skilled doctors can detect signs of corneal infection, inflammation, scarring, and other problems associated with the front structure of the eye using the latest instruments and advanced diagnostic technology. They have been specially trained in all conditions and treatment related to the cornea and ocular surface.
Dry Eye
Dry Eye is also described by the medical term, keratitis sicca, which means decreased quality or quantity of tears. Keratoconjunctivitis sicca refers to eye dryness affecting both the cornea (the clear focusing portion of the front surface of the eye where light enters) and the conjunctiva (the thin, moist membrane that covers the white of the eye).
Patients often experience irritating symptoms and can suffer from more serious vision damage if this condition is left untreated. It is important for patients with this condition to take special care of their eyes in order to alleviate symptoms and prevent complications. Your specialist can diagnose this condition after a thorough evaluation of your eye and tear production using a Schirmer tear test. We have several options available to treat dry eyes.